Sacral Neuro Modulation (SNM) Expertise of Dr. Yasir Iqbal Lone
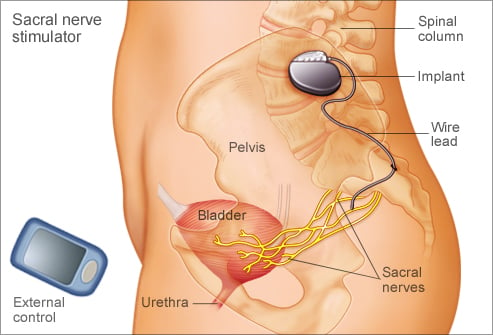
Sacral Neuromodulation (also known as sacral nerve stimulation, or SNS) is a minimally invasive treatment for urinary and bowel dysfunctions. It involves delivering mild electrical impulses to the sacral nerves (usually S3), which help regulate bladder, bowel, and pelvic floor function.
✅ Conditions Treated by SNM
🔍 1. Overactive Bladder (OAB)
Symptoms:
Urgency: Sudden, uncontrollable urge to urinate
Frequency: Needing to urinate more than 8 times per day
Urge incontinence: Leakage of urine following a strong urge
How SNM Helps:
SNM modulates the abnormal communication between the bladder and the brain.
It helps restore normal storage signals, reducing urgency and frequency.
Particularly useful for patients who cannot tolerate or respond to anticholinergic or beta-3 agonist medications.
💧 2. Urinary Urge Incontinence
Definition:
Involuntary leakage of urine preceded by an intense urge to urinate.
SNM Role:
Restores neurological balance between inhibitory and excitatory bladder signals.
Reduces involuntary bladder contractions, thereby decreasing or eliminating episodes of incontinence.
🛑 3. Non-Obstructive Urinary Retention
Definition:
Inability to empty the bladder without any mechanical blockage (like stones, tumors, or strictures).
SNM Role:
Stimulates the sacral nerves to enhance detrusor muscle activity.
Helps improve coordination between the bladder and sphincter, allowing better emptying.
Can reduce or eliminate the need for intermittent self-catheterization (ISC) in many patients.
💩 4. Fecal (Bowel) Incontinence
Symptoms:
Involuntary leakage of stool or gas due to poor sphincter control or nerve dysfunction.
How SNM Helps:
Modulates signals to the anal sphincter and pelvic floor muscles.
Improves sphincter tone and enhances sensory awareness of rectal filling.
Reduces frequency and severity of incontinence episodes in most patients.
🤕 5. Chronic Pelvic Pain Syndrome / Painful Bladder Syndrome (IC/BPS)
(Off-label or in selected cases)
Symptoms:
Pelvic pain, pressure, or discomfort often associated with urinary urgency/frequency.
Diagnosed when no infection or clear cause is present.
SNM Role:
Though not FDA-approved specifically for this indication, SNM can help by:
Modulating sensory nerve activity.
Improving bladder compliance and reducing urgency-related pain.
📉 6. Neurogenic Bladder (Selective cases)
Seen in:
Multiple sclerosis (MS)
Spinal cord injury (SCI) (incomplete lesions)
Parkinson’s disease, etc.
SNM Role:
In some carefully selected patients with incomplete neurological lesions, SNM can:
Improve bladder control
Reduce reflex incontinence
Improve quality of life
🔹 Note: Patients with complete spinal cord injury or severe peripheral nerve damage may not benefit due to lack of viable nerve communication.
⚙️ How the Procedure Works
✅ Stage 1: Test Stimulation (Trial Phase)
Also called Percutaneous Nerve Evaluation (PNE) or Stage 1 Trial.
🎯 Purpose:
To determine if SNM will work for the patient before committing to a permanent implant.
🔧 Procedure Steps:
Local Anesthesia: The area in the lower back near the sacrum is numbed.
Lead Placement:
A thin electrode (test lead) is inserted through the skin into the sacral foramen (usually S3).
Fluoroscopy (X-ray guidance) is used for precise placement.
Connection to External Stimulator:
The test lead is connected to a small external pulse generator, which the patient wears on a belt.
The device delivers mild electrical pulses to the sacral nerve.
Testing Period:
Typically lasts 3 to 14 days.
Patients track improvement in symptoms (e.g., fewer bathroom visits, less leakage).
✅ Success Criteria:
If symptoms improve by 50% or more, the patient is considered a good candidate for permanent implantation.
🧠 Stage 2: Permanent Implantation
If the trial phase is successful, the patient proceeds to the permanent SNM implant.
🛠️ Procedure Steps:
Anesthesia:
Local, regional, or general anesthesia is used depending on the patient and surgeon preference.
Permanent Lead Placement:
A longer, more durable lead is placed into the same sacral foramen as the test lead.
Leads are tunneled under the skin to connect to the neurostimulator.
Neurostimulator Implantation:
A small pulse generator (neurostimulator) is implanted under the skin in the upper buttock (gluteal region).
Device Programming:
After surgery, the device is turned on and custom-programmed using a handheld device.
Stimulation intensity and patterns are adjusted based on symptom relief and patient comfort.
🧠 How It Helps
The stimulation modulates the abnormal nerve signals between the brain, bladder, and bowel. It helps:
Reduce urgency and frequency
Improve continence
Restore voluntary control over voiding and defecation
📊 Effectiveness
70–80% success rate in patients with overactive bladder or urinary incontinence
Long-term satisfaction is high (>80% in many studies)
Reduces reliance on medications with side effects
⚠️ Risks & Considerations
Infection (rare)
Lead migration or breakage
Pain or discomfort at the implant site
Device malfunction
MRI compatibility (older devices are not MRI-safe; newer ones are)
🔄 Reversibility & Maintenance
The procedure is fully reversible — the device can be turned off or removed if ineffective or if complications arise.
Battery life varies:
Rechargeable devices: Up to 15 years
Non-rechargeable devices: 3–7 years, then replacement is needed
Patient Feedback
Read what our satisfied patients say about Dr. Yasir Iqbal Lone.
Dr. Lone provided exceptional care during my surgery. Highly recommend his services!
John Smith
New Delhi
I am thoroughly impressed with Dr. Lone's expertise and caring nature. His staff is friendly, and I felt well taken care of throughout my treatment journey.
Emily Clark
Delhi NCR
